Vitamin C Dose For Gingivitis
PERIODONTITIS AND OXIDATIVE STRESS
Periodontitis is a chronic inflammatory disease caused by our body's immune response to pathogenic bacteria. Periodontitis results in a loss of connective tissue and alveolar bone supporting the teeth and when left untreated, will often result in tooth mobility, pain, swelling and the eventual loss of the involved teeth. The destruction of periodontal tissues is mediated through the production of inflammatory mediators released from immune cells following stimulation by bacterial antigens. Specifically, leukocytes create oxidative stress through production of reactive oxygen species (ROS), which also stimulate the release of enzymes and defensins that degrade the bacterial pathogens during phagocytosis. Because oxidative stress can be modulated by diet,1 investigators have studied if specific dietary antioxidants, particularly vitamin C, are associated with lower risk of periodontal disease or if supplementation with vitamin C can attenuate periodontal disease progression or may be associated with periodontal healing. The relationship between periodontal health and vitamin C as a possible adjunct for periodontal healing will be discussed below.
VITAMIN C IS IMPORTANT FOR PERIODONTAL HEALTH
Vitamin C supports periodontal health through maintenance of gingiva, periodontal ligament, cementum and alveolar bone, which all support teeth. This is partly due to the essential role of vitamin C for the synthesis of collagen. In addition to this role, vitamin C may lower the risk of periodontal disease, and even facilitate healing of the periodontium due to its strong antioxidant capacity that allows it to inactivate ROS that damage structure and function of tissues. Before discussing specific findings about vitamin C and periodontal health, let's first review current recommendations regarding vitamin C intakes and overall vitamin C status of Canadians.
Table 1

HOW MUCH VITAMIN C SHOULD WE CONSUME FOR GENERAL HEALTH?
Consuming a diet rich in fruits and green vegetables provides most of us with the recommended levels of vitamin C. Unlike fat-soluble vitamins such as vitamins A, D, E and K that are stored in fat tissue, vitamin C is water-soluble and not stored in the body. Excess vitamin C is excreted in the urine. Therefore, a continuous supply of vitamin C is required to ensure sufficient levels are available for metabolic processes and target tissues. Most Canadians do not consume fruits and vegetables at the recommended seven to eight servings for women or eight to 10 servings for men.2 This does not mean that most Canadians are vitamin C deficient, but that consuming fruits and vegetables provides us with a variety of vitamins, minerals and fiber that may help reduce the risk of heart disease and some types of cancer.3
According to Health Canada, eating the recommended servings of fruits and vegetables from Canada's Food Guide will help healthy individuals meet the recommended intake for vitamin C.4 Specifically, to maintain near-maximum neutrophil concentrations with minimal urinary excretion of vitamin C, Health Canada recommends that healthy males and females consume 90 mg or 75 mg of vitamin C per day, respectively. As shown in Table 1, consuming even two servings of a variety of commonly-consumed foods in Canada contain the daily recommended level of vitamin C. For this reason, it is not surprising that vitamin C deficiency – of which symptoms include periodontal inflammation, periodontal pain and poor wound healing5 – is rare in Canada. Findings from the Canadian Health Measures Survey (CHMS) showed that fewer than 3% of Canadian adults had vitamin C deficiency.6 Of note was that the prevalence of deficiency was higher among people who rarely or never consumed citrus fruit (13%), those who rarely or never drank 100% fruit juice (7%), and smokers (10%). Not surprisingly, deficiency was not observed in any individuals who took vitamin C-containing supplements.
Due to the potential antioxidant effects of vitamin C there is considerable interest in whether higher than recommended levels of vitamin C are associated with better periodontal health or may support healing of periodontal tissues after specific procedures such as deep scaling and root planing, also called "sanative therapy". Before discussing the findings from those studies, it is important to consider the vitamin C needs of smokers – a group that is particularly at risk for periodontal disease.
SMOKERS NEED MORE VITAMIN C THAN NON-SMOKERS
Smokers have substantially lower levels of serum vitamin C than non-smokers.7 Thus, in combination with the tissue
destruction directly caused by oxidant stress generated through smoking, poor vitamin C status may further exacerbate periodontal disease. The oxidative stress caused by smoking suggests that vitamin C intakes should be higher in smokers. The Food and Nutrition Board suggests that smokers modify their diet to include an additional 35 mg/day of vitamin C.8 This "extra" vitamin C is not difficult to obtain through the diet; a serving of strawberries or raspberries with cereal or yogurt may help smokers get the added vitamin C they need.
RELATIONSHIP BETWEEN VITAMIN C INTAKE AND PERIODONTAL DISEASE
Vitamin C intakes below recommended levels are not likely to directly cause periodontal disease, however, some human studies have shown that patients with severe periodontitis have lower vitamin C intake (<47mg/day)9,10,11,12 or lower plasma vitamin C when compared to healthy controls (8.3 versus 11.3 mg/l, respectively).13 The exact mechanisms through which low plasma vitamin C levels are related to the development or severity of periodontal disease are still being investigated.
It is known that during times of infection and following surgery, there can be a decrease in blood plasma vitamin C levels where additional vitamin C is required for tissue regeneration.14 This is because vitamin C is essential to the formation of new connective tissue in a healing wound and plays an important role in the synthesis of collagen. New tissue is rebuilt around a collagen framework and the enzymes required to form collagen cannot function without vitamin C.
One study used a grapefruit intervention as a means of increasing vitamin C intakes in individuals with chronic periodontitis. Specifically, 58 males and females (including both smokers and non-smokers) with chronic periodontitis, were randomized to two grapefruits per day for two weeks or no intervention. Plasma vitamin C levels were elevated with the grapefruit intervention and had positive effects on reduced gingival bleeding for the non-smokers compared to baseline but no significant clinical improvement with respect to probing depth and plaque index was observed.15 The daily consumption of two grapefruits equated to approximately 185 mg of vitamin C – higher than the current recommended daily allowance (RDA) for vitamin C for healthy individuals; it is also important to note that other sources of vitamin C and micronutrients were not reported in this study.
A small intervention study was conducted amongst two groups (n= 15 per group) of non-smoking patients suffering from chronic periodontitis.16 Each group was treated with scaling and root planing but the intervention group was supplemented with 2 g/day vitamin C for four weeks post-therapy. It is of interest to note that both groups' plasma total antioxidant capacity significantly increased following therapy to equal baseline levels of healthy control subjects. However, the vitamin C supplementation itself did not result in a measurable clinical benefit. This finding is supported by another study that demonstrated that scaling and root planing alone was able to reduce oxidant stress (measured as an increase in the ratio of reduced glutathione to oxidized glutathione) in patients with chronic periodontitis for up to three but not six months following treatment. Moreover, the authors suggest that providing micronutrients with antioxidant activity, such as vitamin C, may normalize oxidant stress after scaling and root planing over the long-term.17 Also, because antioxidants such as vitamin C may act synergistically with other nutrients, it is possible that a food source may be more effective. Interestingly, a recent Canadian study determined that a higher intake of vitamin C from foods but not from supplements was associated with improved healing after deep scaling and root planing.18 Moreover, this relationship was found only when non-smokers were studied; this same association was not present in smokers, perhaps due to the overwhelming detriment of smoking on periodontal healing. Intakes of 5 or more servings of fruits and vegetables/day by non-smokers was shown to be associated with a significantly lower percentage of sites with probing depths >3 mm eight weeks following non-surgical scaling and root planning compared to patients with lower dietary intakes of fruits and vegetables (1.5 to 5 servings/day). Also, dietary vitamin C intakes greater than 150 mg/day were associated with a better response to sanative therapy, suggesting that intake of vitamin C beyond the RDA of 75 or 90 mg/day may be beneficial in periodontal treatment, but cause and effect remains to be determined. Coincidently, the association between dietary intake of vitamin C and reduction in probing depth was attenuated when total vitamin C intake (dietary and supplement source of vitamin C) was assessed. This finding suggests that the synergistic effect of whole foods rather than supplements may offer a more robust approach to periodontal healing outcomes. However, well-designed, long-term studies involving a whole food approach are needed determine whether a 'cause and effect' relationship exists between higher vitamin C intakes and improved periodontal health.
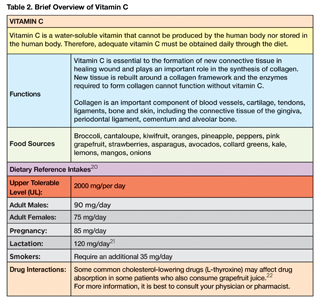
Table 2
SHOULD INDIVIDUALS WITH PERIODONTAL DISEASE USE VITAMIN C SUPPLEMENTS?
There is currently insufficient scientific evidence to recommend the use of vitamin C supplements to manage periodontal disease or facilitate healing after periodontal procedures. However, ensuring individuals consume the appropriate number of servings of fruits and vegetables will provide higher than recommended levels of vitamin C and is important for overall health.
KEY POINTS:
While there are many outlets in the media and online claiming that vitamin C can cure periodontal disease, these claims are not substantiated by existing scientific evidence. In fact, neither consumption of foods rich in vitamin C nor supplementation with vitamin C will cure periodontal disease but may favourably modulate the host inflammatory response and support health of the periodontium.
• Because smoking induces oxidative stress, smokers require an additional 35 mg vitamin C/day
• Patients who consume the recommended seven to 10 daily servings of fruits and vegetables will likely meet the RDA for vitamin C
• Current evidence is insufficient to support recommendation of vitamin C supplementation for the treatment of periodontal disease
ADVICE FOR PATIENTS:
• Eating an orange or ½ cup of sweet peppers a day is usually enough to receive the recommended level (RDA) of
vitamin C but it is recommended that seven to 10 servings of fruits and vegetables are consumed each day, with a variety of colours, as per Canada's Food Guide (available at www.canada.ca/en/health-canada/services/canada-food-guides.html) for optimal overall health
• Vitamin C rich foods are best consumed daily. Raw or minimally processed or cooked sources will contain higher levels of vitamin C for maximal potential benefit
• Enjoy citrus fruits and juice but choose fruit more often than juice
Juice has the potential to quickly spike blood sugar levels and will likely have more sugar and less fibre than eating fruit in its whole form
• Supplemental vitamin C may only be required when patients are not receiving enough from their diet
o Patients should read labels closely for vitamin C dosages and use only as directed after consultation with their physician or a dietitian.
o Typical levels of vitamin C in a one-a-day multivitamin can range from 60 mg to 120 mg or higher
o Vitamin C is generally considered to be non-toxic, however intakes above the Upper Tolerable level (UL) of 2000 mg/day are not associated with proven health benefits and may cause harm (i.e. gastrointestinal distress, increased risk of kidney stones or impaired absorption of vitamin B12). OH
Oral Health welcomes this original article.
References
- Chapple, I.L. (2009). Potential mechanisms underpinning the nutritional modulation of periodontal inflammation. Journal of American Dental Association. 1402: 178-184.
- Statistics Canada. (2017). Fruit and Vegetable Consumption, 2015. Available at: http://www.statcan.gc.ca/pub/82-625-x/2017001/article/14764-eng.htm
- Pérez, C.E. (2002). Fruit and vegetable consumption. Health Reports. Statistics Canada, Catalogue no. 82-003. 1 (3).
- Health Canada. (2011). Eating well with Canada's food guide (HC Pub.: 4651). Ottawa: Queen's Printer.
- Grosso, G., Bei, R., Mistretta, A., et al. (2013). Effects of vitamin C on health: a review of evidence. Frontiers in Bioscience. 18: 1017-29.
- Statistics Canada. Canadian Health Measures Survey (CHMS). Detailed Information for January 2012 to December 2013 (Cycle 3) . Available at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=5071
- Schetcman, G., Byrd, J.C., Gruchow, H.W. (1989). The influence of smoking on vitamin C status in adults. American Journal of Public Health. 79(2):158-62.
- Institute of Medicine, Food and Nutrition Board. (2000). Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. National Academy Press. Washington, DC.
- Lee J-H, Shin M-S, Kim E-J, Ahn Y-B, Kim H-D (2017) The association of dietary vitamin C intake with periodontitis among Korean adults: Results from KNHANES IV. PLoS ONE. 12(5): e0177074.
- Chapple, I.L., Milward, M.R., Dietrich, T. (2007). The prevalence of inflammatory periodontitis is negatively associated with serum antioxidant concentrations. Journal of Nutrition. 137:657–64.
- Iwasaki, M., Manz, M.C., Taylor, G.W., Yoshihara, A, Miyazaki, H. (2012). Relations of serum ascorbic acid and alpha-tocopherol to periodontal disease. Journal of Dental Research. 91:167–72.
- Nishida, M., Grossi, S.G., Dunford, R.G., Ho, A.W., Trevisan, M. (2000). Dietary vitamin C and the risk for periodontal disease. Journal of Periodontology. 71(8):1215–1223
- Kuzmanova, D., Jansen, I.D., Schoenmaker, T., Nazmi, K., Teeuw, W.J., Bizzarro, S., Loos, B.G., van der Velden, U. (2012). Vitamin C in plasma and leukocytes in relation to periodontitis. Journal of Clinical Periodontology. 39: 905–12.
- Irvin, T.T. (1982). Vitamin C requirements in postoperative patients. International Journal for Vitamin and Nutrition Research. 23:277-86.
- Staudte, H., Sigusch, B.W., Glockmann, E. (2005). Grapefruit consumption improves vitamin C status in periodontitis patients. British Dental Journal. 199(4): 213-7.
- Abou Sulaiman, A.E.; Shehadeh, R.M. (2010). Assessment of total antioxidant capacity and the use of vitamin C in the treatment of non-smokers with chronic periodontitis. Journal of Periodontology. 81; 1547–1554.
- Palwankar, P., Rana, M., Arora, K., & Deepthy, C. (2015). Evaluation of non-surgical therapy on glutathione levels in chronic periodontitis. European Journal of Dentistry. 9(3), 415–422.
- Dodington, D., Fritz, P., Sullivan, P., Ward, W. (2015). Higher Intakes of Fruits and Vegetables, b-Carotene, Vitamin C, a-Tocopherol, EPA, and DHA Are Positively Associated with Periodontal Healing after Nonsurgical Periodontal Therapy in Nonsmokers but Not in Smokers. Journal of Nutrition and Disease. 45:2512–9.
- Zeng, Chuli. (2013). Effects of different cooking methods on the vitamin C content of selected vegetables. Nutrition & Food Science. 43:438-443.
- Health Canada. Dietary Intake Reference Tables. Retrieved on 15 July 2017 from https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/hpfb-dgpsa/pdf/nutrition/dri_tables-eng.pdf
- Institute of Medicine, Food and Nutrition Board. (2000). Dietary Reference Intakes for Vitamin C, Vitamin E, Selenium, and Carotenoids. National Academy Press. Washington, DC.
- Bailey, D.G. (2010). Fruit juice inhibition of uptake transport: a new type of food-drug interaction. British Journal of Clinical Pharmacology. 70(5):645-55.
 Stephanie Klok is a registered dental hygienist working at a periodontal specialty clinic with over eight years of experience in the dental field. She is currently completing the first year of her Master's degree in Applied Health Sciences at Brock University. Her research focuses on the role that nutrition plays on periodontal healing following sanative therapy.
Stephanie Klok is a registered dental hygienist working at a periodontal specialty clinic with over eight years of experience in the dental field. She is currently completing the first year of her Master's degree in Applied Health Sciences at Brock University. Her research focuses on the role that nutrition plays on periodontal healing following sanative therapy.
 Peter Fritz is a certified specialist in Periodontics in Fonthill, Ontario. His translational research program investigates optimal collaborative strategies for periodontal wellness throughout the lifecycle involving nutrition, advanced instrumentation, microsurgery and tissue regeneration.
Peter Fritz is a certified specialist in Periodontics in Fonthill, Ontario. His translational research program investigates optimal collaborative strategies for periodontal wellness throughout the lifecycle involving nutrition, advanced instrumentation, microsurgery and tissue regeneration.
 Wendy Ward is a Professor and Canada Research Chair in the Department of Kinesiology in the Faculty of Applied Health Sciences at Brock University. Her research program investigates how early diet sets a trajectory for a stronger, healthier skeleton at adulthood, and also how diet can support bone health at older life stages. Within this research program, a number of novel foods and food components are studied: vitamin D, soy and its isoflavones, omega-3 fatty acids in flaxseed and fish oil, and tea and its flavonoids.
Wendy Ward is a Professor and Canada Research Chair in the Department of Kinesiology in the Faculty of Applied Health Sciences at Brock University. Her research program investigates how early diet sets a trajectory for a stronger, healthier skeleton at adulthood, and also how diet can support bone health at older life stages. Within this research program, a number of novel foods and food components are studied: vitamin D, soy and its isoflavones, omega-3 fatty acids in flaxseed and fish oil, and tea and its flavonoids.
RELATED ARTICLE: The New Canada Food Guide: Considerations For Periodontal Health
Source: https://www.oralhealthgroup.com/features/vitamin-c-update-implications-periodontal-health-healing/

0 Komentar